Degenerative disc disease (osteochondrosis) in the thoracic spine is a relatively rare condition compared to other spines. This is because the rib cage stabilizes the thoracic vertebrae, limiting movement and constant flexion and extension injuries, as occurs in the rest of the spine. If osteochondrosis develops in the thoracic spine, most often its development is associated with trauma.

Degeneration, destruction, and inflammation in the disc area can cause a variety of symptoms, depending on the severity of the problem. Disc pathology can lead to symptoms such as decreased range of motion in the back, back pain that can radiate into the intercostal space, numbness, tingling, muscle spasm, or certain combinations of these symptoms. The most common manifestations of osteochondrosis in the thoracic region occur at the T8-T12 level. As a rule, the manifestations of osteochondrosis in the thoracic region are: protrusion, extrusion of the disc, herniated disc with sequestration, spondylolisthesis.
Treatment of osteochondrosis of the thoracic spine is usually conservative, but in the presence of complications such as compression of the spinal cord, surgical treatment is possible.
Osteochondrosis (degenerative disc disease) is not actually a disease, but rather a term used to describe the progressive changes in the discs associated with progressive wear and the development of symptoms secondary to disc degeneration. Disc degeneration is a normal involutional process, but in certain situations, the degeneration process can accelerate, for example, as a result of trauma, overuse, and musculoskeletal imbalances such as scoliosis. Disc degeneration itself is not a problem, but the conditions associated with it can lead to the development of advanced symptoms.
Stages of disc degeneration
The progression of disc degeneration can be classified into the following stages:
Dysfunction
- Tears are possible in the area of the annulus fibrosus, with irritation of the facet joints at the corresponding level of the spine.
- Loss of joint mobility, local low back pain, muscle spasm and limitations in trunk mobility, especially extension.
Instability
- Loss of fluid from a disc with dehydration and decreased disc height. Weakness of the facet joints and capsules may develop, leading to instability.
- The patient will experience stabbing pain, straightening of the spine, and a sharp decrease in range of motion in the trunk.
Re-stabilization
- The human body reacts to instability by forming additional bone formations in the form of osteophytes that, to some extent, help stabilize the spine. But too much bone formation can lead to spinal stenosis.
- Back pain usually decreases but remains less severe. Some people may develop symptoms similar to those of stenosis.
The reasons
- Involutive changes in the body are the most common cause of disc degeneration. As the body ages, the discs gradually lose their liquid portion and become dehydrated. The discs begin to narrow and lose their height, which affects their ability to absorb shock and stress.
- The outer annular fibrous structures of the disc can begin to crack and rupture, weakening the walls of the disc.
- People who smoke, are obese, and participate in strenuous activities are more likely to experience disc degeneration.
- An injury to the spine or disc from a fall or impact can trigger the degeneration process.
- A herniated disc can initiate the development of disc degeneration.
- Unlike muscles, discs have minimal blood flow, so they have no reparative capacity.
Symptoms
The symptoms associated with osteochondrosis of the thoracic spine will depend on the location and structures involved in this process. Disc degeneration in the thoracic spine can affect the back, the area under the scapula, or along the ribs.
- Many patients with degenerative disc disease of the thoracic spine may have no symptoms.
- Chronic chest pain with / without radiation to the ribs.
- Sensory changes such as numbness, tingling or paresthesia in cases of nerve compression.
- Muscle spasm and posture changes in the thoracic back.
- Loss of range of motion, with reduced ability to move the trunk, especially when turning or leaning to one side.
- Sitting for long periods can cause back pain and arm pain.
- Difficulty lifting weights and raising your arms above your head.
- In later stages, spinal stenosis can develop, leading to weakness in the lower extremities and loss of coordination of movements. In these cases, surgery will be required.
Diagnostics
In addition to performing a comprehensive exam, the doctor may order the following tests to verify the diagnosis:
- Bone scan,helps determine if there is joint degeneration, fractures, bone malformations, arthritis, tumors, or infection.
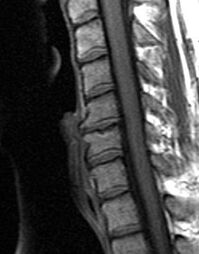
- Magnetic resonanceto determine morphological changes in soft tissues, including visualization of discs, spinal cord, and nerve roots.
- Computed tomographya scan that can provide cross-sectional images of structures in the spine.
- EMG,This diagnostic method is used to determine nerve damage and the level of damage.
- MyelogramAs a general rule, this research method is necessary to clarify morphological changes in the degree of impact on the roots and spinal cord and to plan surgical intervention.
Treatment
Treatment of osteochondrosis of the thoracic spine will depend on the severity of the condition.
Treatment of acute pain syndrome:
- Rest: Avoid activities that cause pain (bending over, standing up, twisting, twisting, or reaching backward).
- Medications to reduce inflammation (anti-inflammatories and pain relievers).
- Ice in acute cases can relieve spasms, relieve pain.
- Local exposure to heat can help relieve pain and muscle tension.
- Light gymnastic exercises to eliminate biomechanical disorders associated with osteochondrosis and improve joint mobility, normal spinal configuration, posture and range of motion.
- It may be necessary to wear a brace to relieve stress on the facet joints and the muscles of the thoracic spine.
- Corticosteroids are used to reduce inflammation in moderate to severe cases.
- Epidural injections directly into the damaged disc area.
In mild cases, the use of topical cold medications may be enough to relieve pain. After pain relief, physical therapy and exercises are recommended to stretch and strengthen the back muscles. The return to normal activity should be gradual to prevent recurrence of symptoms.
The main conservative methods of treatment of osteochondrosis of the thoracic spine.
Drug treatment
The task of using drugs in the treatment of osteochondrosis of the thoracic spine, especially in acute pain syndrome, is to reduce pain, inflammation and muscle spasms.
- Over-the-counter medications for mild to moderate pain.
- Narcotic pain relievers for severe pain that cannot be controlled with other treatment methods.
- Muscle relaxants to reduce acute muscle spasm.
- Prescription pain relievers.
- Injections such as facet joint injections, locks, or epidural injections. These may include injecting corticosteroids into specific areas to reduce local inflammation.
- Manual therapies, including soft tissue massage, stretching and mobilization of the joints performed by a specialist, improve the geometry, mobility and range of motion in the thoracic spine. The use of mobilization techniques also helps to modulate pain.
- Exercise therapy (therapeutic exercises), including stretching and muscle strengthening exercises, to restore range of motion and strengthen the muscles of the back and abdomen, supporting, stabilizing, and reducing stress on the discs and back. An exercise program, especially exercises with weights or weights, should be started after pain, muscle spasms, and swelling have subsided. An incorrectly selected exercise program can aggravate symptoms. Therefore, the selection of exercises should be done with a doctor who specializes in physical therapy.
- Neuromuscular retraining to improve posture, restore stability, teach the patient the correct biomechanics of movement to protect damaged discs and spine.
- Physical therapy, which includes the use of ultrasound, electrical stimulation, and cold lasers, helps reduce pain and inflammation of the spinal structures.
- Home exercise programs, including muscle strengthening, stretching and stabilization exercises, and lifestyle changes to reduce stress on the spine.
- Acupuncture. This method of treatment can be used in the presence of sensory disturbances or to restore conduction and reduce pain.
Surgical treatments
Most hernias located in the thoracic spine of the thoracic disc can be successfully treated without surgery. However, when conservative treatment of osteochondrosis of the thoracic spine is ineffective, surgery may be recommended, especially if the patient exhibits some of the following symptoms:
- Increased radicular pain.
- Increased pain and nerve damage.
- Development or increase of muscle weakness.
- Increased numbness or paresthesia.
- Loss of control of bowel and bladder function.
The most common surgery associated with disc degeneration is discectomy, in which the disc is removed through an incision. However, there are several surgical procedures that may be recommended in cases of osteochondrosis and disc degeneration. The choice of surgical method depends on the cause of the symptoms. Basic surgical techniques: include foraminotomy, laminotomy, spinal laminectomy, spinal decompression, and spinal fusion.
Forecast
Most of the problems associated with osteochondrosis of the thoracic spine can be resolved without surgery and people return to normal work. Osteochondrosis in the thoracic spine due to anatomical stiffness develops less than elsewhere. The duration of treatment, as a rule, does not exceed 4-12 weeks and depends on the severity of the symptoms. Patients should continue with the stretching, strengthening, and stabilization exercise program. A good long-term prognosis requires the use of proper body movements and mechanics and an awareness of the importance of maintaining spinal health.































